The rollout of HIV Pre-Exposure Prophylaxis (PrEP) has had a dramatic positive impact on HIV acquisition since becoming available as part of widespread NHS treatment in 2020 following several years of trials. Yet the data show that not all groups of people have benefited equally. The UK Health Security Agency publish tables annually which provide a detailed breakdown of all individuals with new HIV diagnoses in England, allowing us to both identify trends and determine which groups are underserved. Specifically, these data provide us insight into those communities and groups across England which will benefit from greater outreach and awareness of PrEP as a viable treatment option for the prevention of HIV transmission.
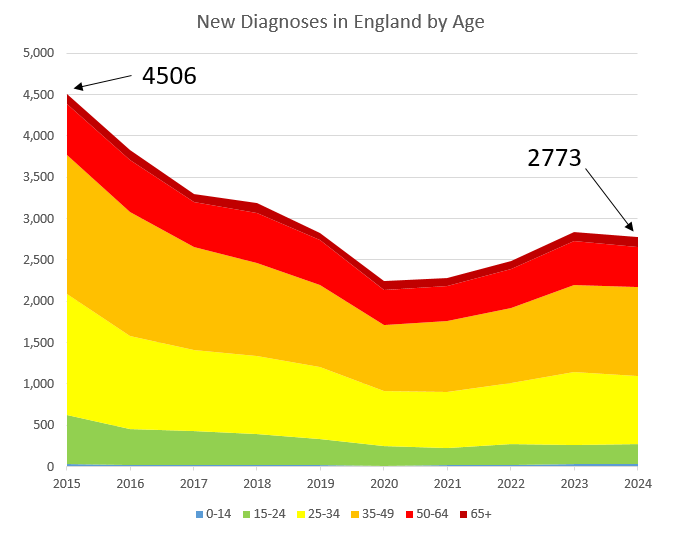
We can see in Figure 1 that the overall incidence of new HIV acquisitions detected in each year from 2015-2024 has declined from a 2015 high of 4,506 new cases to just 2,773 in 2024 – even allowing for a probable dip in overall testing during 2020 and 2021, the first years of the Covid pandemic. There might also be a “rebound factor” at work in the slight increase of 2022-2023: higher incidence in these years might be picking up cases which would have been detected in 2020 or 2021 in the absence of pandemic-associated restrictions. The incidence from 2015-2024 has also fallen in each age group: whilst individuals aged 35-49 have been affected most in each year, the overall trend is clearly downwards:
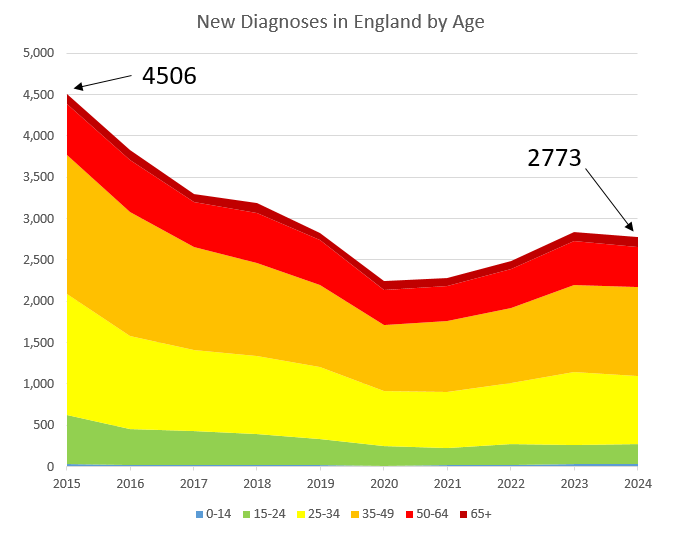
Figure 1: New HIV Diagnoses in England by Age
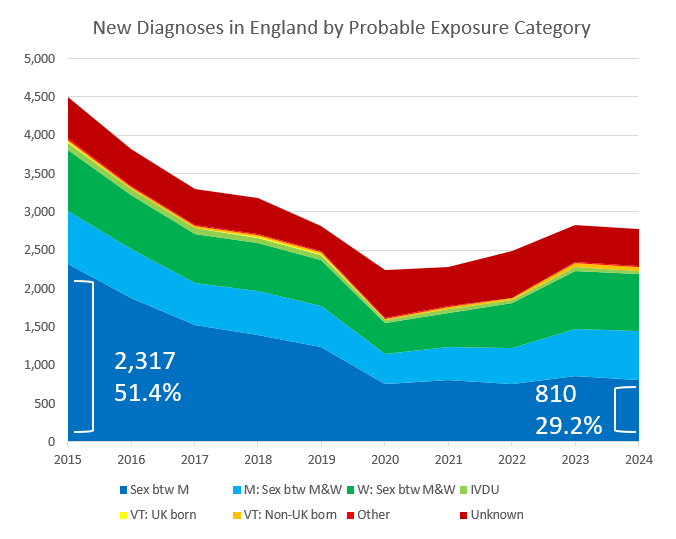
The data in Figure 2, however, tell a different story. As we examine the trends covering modes of transmission, we can see where the PrEP rollout and other interventions are having a large impact – and where they possibly are not. Whilst cases of HIV transmitted via sex between men was 51.4% of all transmissions in 2015, it had fallen to 29.2% of all cases (a smaller proportion of a much smaller number) by 2024. The trends in heterosexual transmission, however, were not quite so affirming. New cases of HIV resulting from opposite-sex contact fell slightly from 2015-2024 in both men and women (690 to 634 and 795 to 749, respectively), but overall percentages of these groups among all new cases rose significantly (15.3% to 22.9% and 17.6% to 27.0%, respectively).
Table 1: New Diagnoses in England by Probable Exposure Category (emphasis added):
| Probable HIV exposure |
2015 |
2024 |
| Sex btw M |
2317 |
810 |
| M: Sex btw M&W |
690 |
634 |
| W: Sex btw M&W |
795 |
749 |
| IVDU |
104 |
32 |
| VT: UK born |
8 |
2 |
| VT: Non-UK born |
27 |
53 |
| Other |
23 |
16 |
| Unknown |
542 |
476 |
| Total |
4506 |
2772 |
|
|
|
| Sex btw M |
51.4% |
29.2% |
| M: Sex btw M&W |
15.3% |
22.9% |
| W: Sex btw M&W |
17.6% |
27.0% |
| IVDU |
2.3% |
1.2% |
| VT: UK born |
0.2% |
0.1% |
| VT: Non-UK born |
0.6% |
1.9% |
| Other |
0.5% |
0.6% |
| Unknown |
12.0% |
17.2% |
| Total |
100.0% |
100.0% |
The data above make it clear that PrEP is effective in reaching patients who identify as GBMSM. It is also worth pointing out that rates among transmission via intravenous drug use (IVDU) and vertical transmission (from mother to baby at childbirth) have fallen from 2015-2024, albeit from very low bases. However, it seems that the message of effective HIV prevention is not percolating through all groups equally.
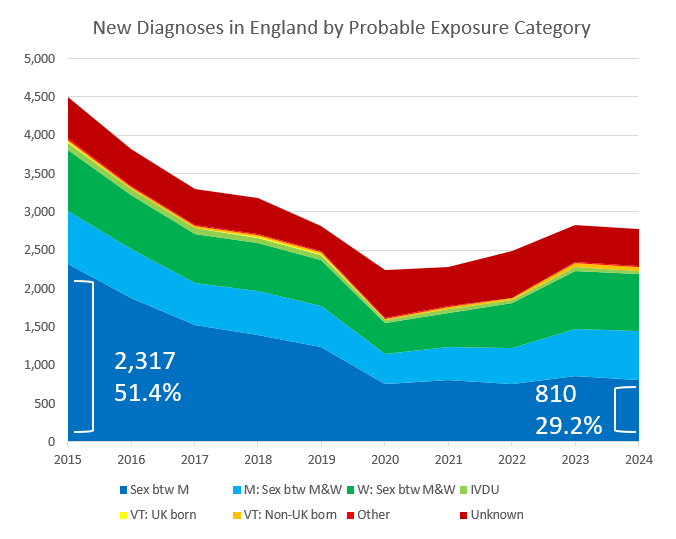
Figure 2: New Diagnoses in England by Probable Exposure Category
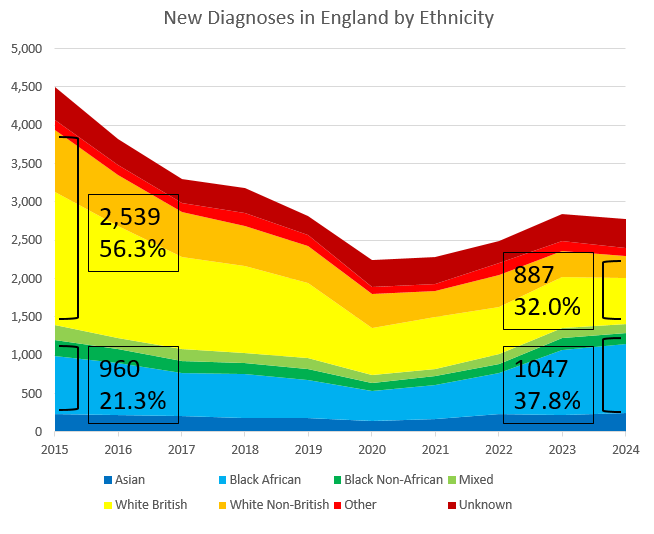
As in Figure 2, the data represented in Figure 3 tell a mixed tale. In 2015, White (British and Non-British) people made up 2,539 of all new HIV diagnoses (56.3% of 4,506), and this number fell to 887 by 2024 (32.0% of a much lower 2,773 new-case count). This is likely a success of the rollout of PrEP and effective PrEP messaging. Black (African and Non-African) patients, however, actually saw an increase of new cases from 2015 to 2024 – rising from 960 (21.3%) of all new diagnoses in 2015 to 1,047 (37.8%) in 2024:
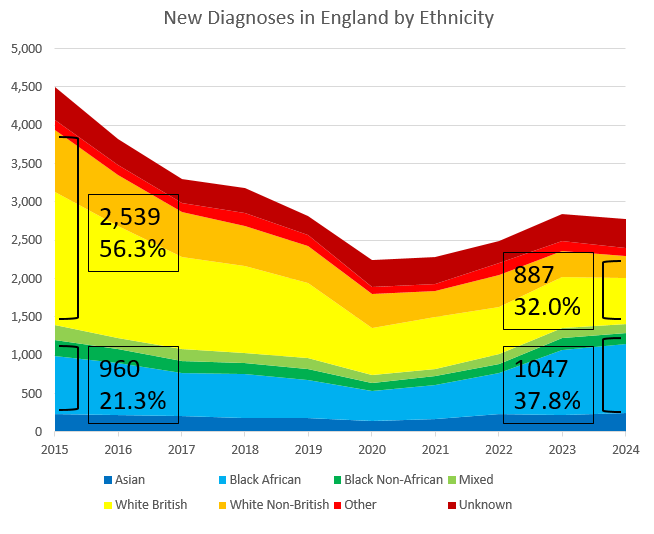
Figure 3: New Diagnoses in England by Ethnicity
Table 2: New Diagnoses in England by Ethnicity (emphasis added):
| Ethnicity |
2015 |
2024 |
| Asian |
240 |
250 |
| Black African |
754 |
894 |
| Black Non-African |
206 |
153 |
| Mixed |
201 |
110 |
| White British |
1726 |
604 |
| White Non-British |
813 |
283 |
| Other |
131 |
103 |
| Unknown |
435 |
376 |
| Total |
4506 |
2773 |
|
|
|
| Asian |
5.3% |
9.0% |
| Black African |
16.7% |
32.2% |
| Black Non-African |
4.6% |
5.5% |
| Mixed |
4.5% |
4.0% |
| White British |
38.3% |
21.8% |
| White Non-British |
18.0% |
10.2% |
| Other |
2.9% |
3.7% |
| Unknown |
9.7% |
13.6% |
| Total |
100.0% |
100.0% |
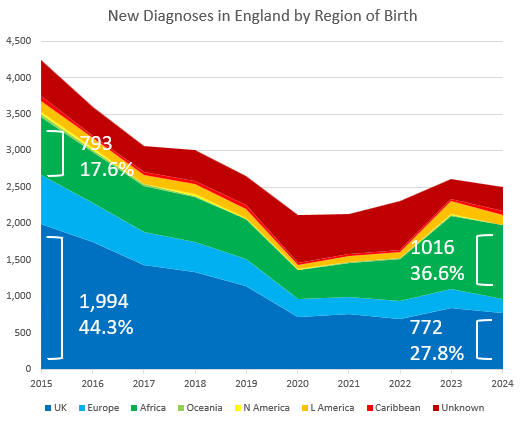
As the data above show, some communities are not as effectively reached by the PrEP message as others. Breaking this down by region of birth shows the same story: whilst new diagnoses of HIV amongst people born in the UK fell from 44.3% to 27.8% of all diagnoses from 2015 to 2024, the number of new diagnoses amongst people born in Africa rose over the same time period both in relative (17.6% to 36.6%) and absolute terms (793 to 1016). More people born in Africa were diagnosed with HIV in England for the first time in 2024 than were in 2015; this absolute increase does not hold for people from any other region in the world.
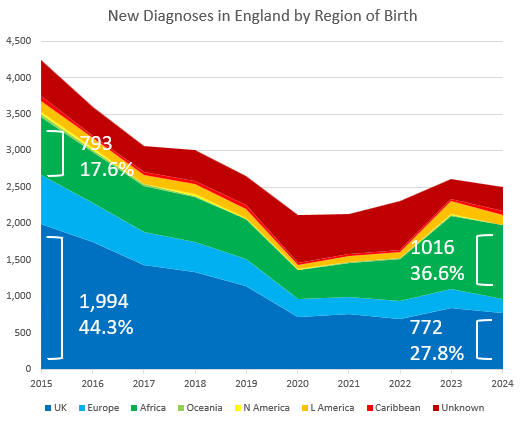
Figure 4: New Diagnoses in England by Region of Birth
Table 3: New Diagnoses in England by Region of Birth (emphasis added):
| Region of birth |
2015 |
2024 |
| UK |
1994 |
772 |
| Europe |
676 |
190 |
| Africa |
793 |
1016 |
| Asia |
267 |
267 |
| Oceania |
36 |
6 |
| N America |
39 |
5 |
| L America |
145 |
133 |
| Caribbean |
63 |
52 |
| Unknown |
493 |
332 |
| Total |
4506 |
2773 |
|
|
|
| UK |
44.3% |
27.8% |
| Europe |
15.0% |
6.9% |
| Africa |
17.6% |
36.6% |
| Asia |
5.9% |
9.6% |
| Oceania |
0.8% |
0.2% |
| N America |
0.9% |
0.2% |
| L America |
3.2% |
4.8% |
| Caribbean |
1.4% |
1.9% |
| Unknown |
10.9% |
12.0% |
| Total |
100.0% |
100.0% |
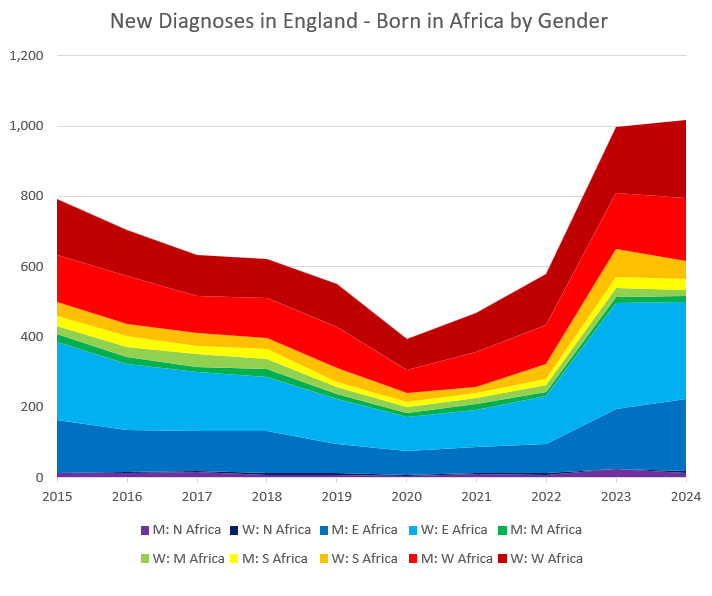
The UK Health Security Agency data actually break the data down even further: we see not only the sex of each individual new HIV diagnosis in each year, but also in which region of Africa (North, East, South, West or Central) each individual was born. The majority of new HIV diagnoses in 2015 and 2024 were from men and women born in East and West Africa; unfortunately, new diagnoses increased in all four of these groups over the interval period:
Table 4: New Diagnoses in England – Born in Africa by Gender (emphasis added):
| Region of birth |
2015 |
2024 |
| M: N Africa |
12 |
13 |
| W: N Africa |
0 |
6 |
| M: E Africa |
152 |
206 |
| W: E Africa |
223 |
274 |
| M: M Africa |
23 |
17 |
| W: M Africa |
22 |
19 |
| M: S Africa |
29 |
29 |
| W: S Africa |
38 |
51 |
| M: W Africa |
134 |
181 |
| W: W Africa |
160 |
220 |
| Total |
793 |
1016 |
|
|
|
| M: N Africa |
1.5% |
1.3% |
| W: N Africa |
0.0% |
0.6% |
| M: E Africa |
19.2% |
20.3% |
| W: E Africa |
28.1% |
27.0% |
| M: M Africa |
2.9% |
1.7% |
| W: M Africa |
2.8% |
1.9% |
| M: S Africa |
3.7% |
2.9% |
| W: S Africa |
4.8% |
5.0% |
| M: W Africa |
16.9% |
17.8% |
| W: W Africa |
20.2% |
21.7% |
| Total |
100.0% |
100.0% |
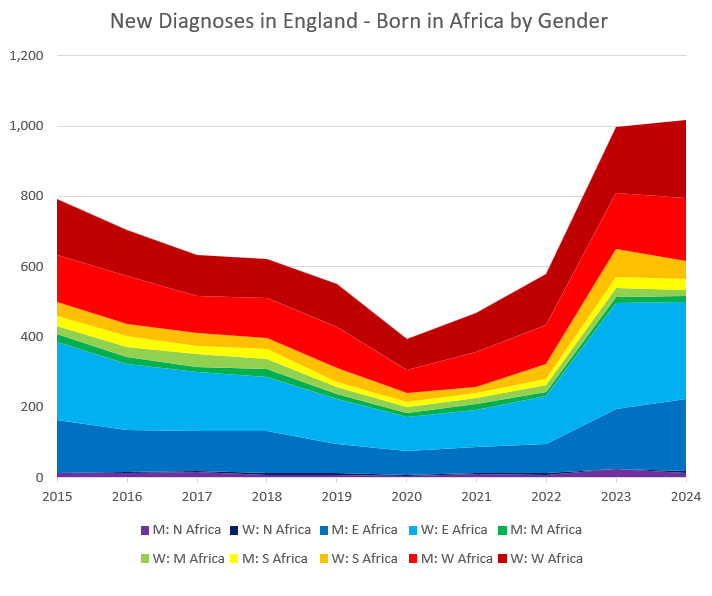
Figure 5: New Diagnoses in England – Born in Africa by Gender
In conclusion, the results are mixed. Whilst the message behind PrEP has enjoyed fantastic success in some communities in England (primarily UK-born, white MSMs), this message appears not to have percolated quite so well through other demographic groups (namely African-born heterosexual men and women). Given our government goal to eliminate all new HIV transmission by 2030 – four short years from now – we have our work cut out for us. And whilst it’s essential to ensure that the PrEP message reaches deeper into under-represented communities as outlined above, we cannot pause the efforts that have shown such success in the groups which have already drawn the most benefit. In short, the battle to stop HIV transmission is showing some early success, but it is far from over.
Sources:
- https://www.gov.uk/government/news/hiv-drug-prep-to-be-available-across-england
- https://www.gov.uk/government/statistics/hiv-annual-data-tables